Euthanasia, also known as mercy killing or assisted suicide, is a highly controversial topic that continues to spark debate among ethicists, healthcare professionals, policymakers, and the general public. One particularly noteworthy case that reignited the euthanasia debate is the tragic story of Jolanda Fun, a 48-year-old woman diagnosed with terminal cancer. Jolanda’s case has brought to light the complexities and ethical dilemmas surrounding euthanasia, shedding light on the moral, legal, and social implications of end-of-life decisions.
Jolanda Fun’s Story
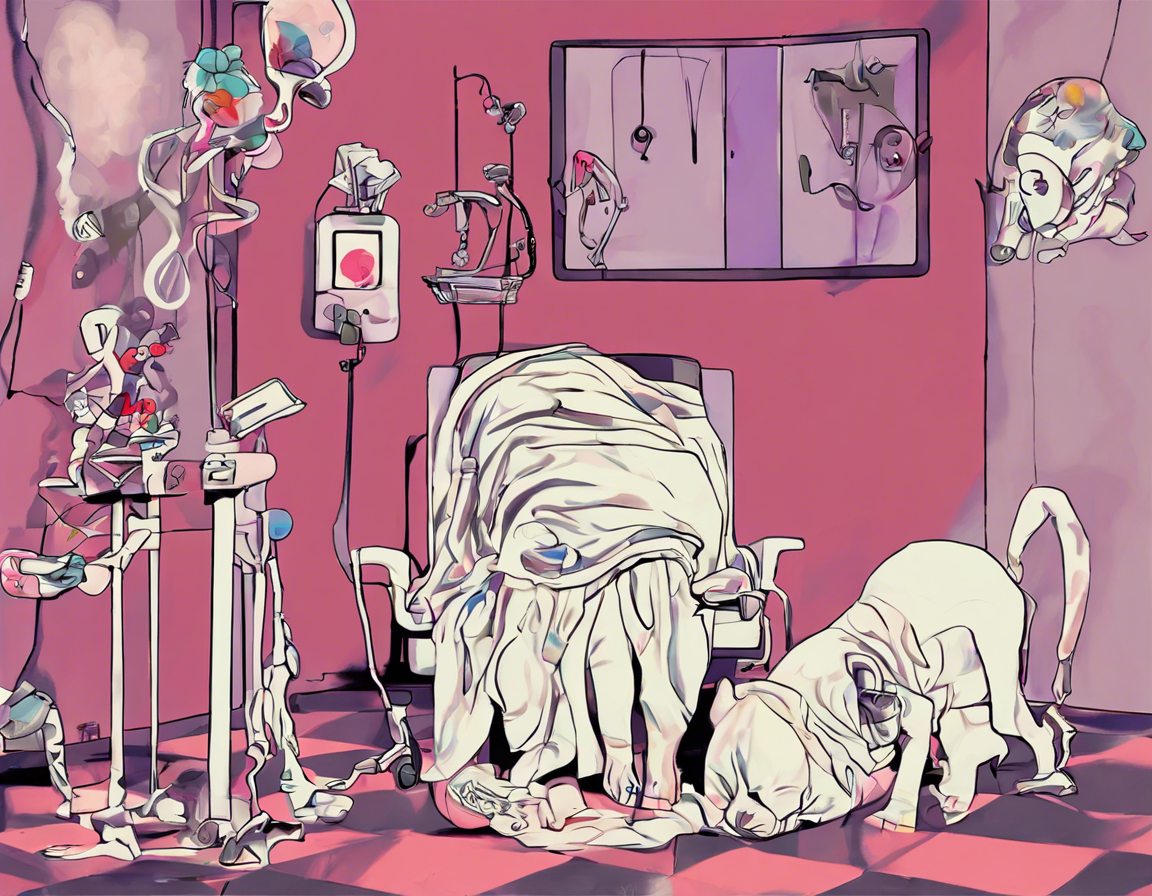
Jolanda Fun was a vibrant and active woman who was diagnosed with an aggressive form of cancer at the age of 46. Despite undergoing various treatments, her condition deteriorated rapidly, and she was faced with excruciating pain and suffering. Jolanda expressed her desire to end her life on her own terms, as she did not want to continue living in unbearable pain and distress.
The case of Jolanda Fun gained widespread media attention as she fought for her right to die with dignity. Her plea for euthanasia sparked a heated debate among supporters and opponents of the practice, with many questioning the ethical and legal implications of her request. Ultimately, Jolanda was able to end her life with the assistance of a physician in a country where euthanasia is legal, highlighting the importance of patient autonomy and end-of-life decision-making.
The Ethics of Euthanasia
The ethical considerations surrounding euthanasia are complex and multifaceted, with proponents arguing that it is a compassionate and humane way to relieve suffering, while opponents raise concerns about the sanctity of life and the potential for abuse. Ethical principles such as autonomy, beneficence, non-maleficence, and justice play a crucial role in shaping the debate over euthanasia.
Autonomy: The principle of autonomy upholds an individual’s right to make decisions about their own body and end-of-life care. Supporters of euthanasia argue that respecting a person’s autonomy means allowing them to choose how and when they want to die.
Beneficence: The principle of beneficence emphasizes the obligation to act in the best interest of the patient and to alleviate their suffering. Proponents of euthanasia argue that ending a patient’s life can be a compassionate act of beneficence in cases of unbearable suffering.
Non-maleficence: The principle of non-maleficence dictates that healthcare providers must not harm their patients and must strive to prevent harm. Opponents of euthanasia raise concerns about the potential for abuse and coercion, highlighting the risk of harm to vulnerable individuals.
Justice: The principle of justice calls for fair and equitable treatment for all individuals, regardless of their circumstances. The debate over euthanasia raises questions about social justice and equal access to end-of-life care options, particularly for marginalized populations.
The Legal Landscape of Euthanasia
The legal status of euthanasia varies significantly around the world, with some countries permitting physician-assisted suicide or voluntary euthanasia under certain circumstances, while others prohibit the practice entirely. In countries where euthanasia is legal, strict regulations and safeguards are in place to ensure that the decision is made voluntarily and with full informed consent.
Netherlands and Belgium are among the few countries that have legalized euthanasia, allowing patients to request medical assistance in dying under specific conditions. In these countries, physicians are permitted to administer life-ending drugs to terminally ill patients who meet the criteria for euthanasia, such as unbearable suffering and a voluntary request.
Switzerland is another notable example where euthanasia is legal under certain circumstances, with organizations such as Dignitas providing end-of-life services to individuals seeking a peaceful death. The legal framework in Switzerland allows for assisted suicide for both residents and non-residents, further contributing to the ongoing debate over euthanasia tourism and cross-border end-of-life care.
The Role of Healthcare Professionals
Healthcare professionals play a critical role in end-of-life care and the euthanasia debate, as they are often called upon to provide palliative care and support to terminally ill patients. Physicians, nurses, and other healthcare providers must navigate the ethical and legal complexities of euthanasia while upholding their professional obligations and ethical responsibilities.
Palliative care focuses on improving the quality of life for patients with serious illnesses, offering pain management, symptom relief, and emotional support to enhance comfort and well-being. Advocates of palliative care argue that comprehensive and compassionate end-of-life care can alleviate the suffering of patients and families, potentially reducing the need for euthanasia.
Advance care planning and advance directives are essential components of end-of-life care, allowing individuals to express their treatment preferences and medical wishes in advance. By discussing care options and goals of care with patients, healthcare professionals can facilitate advance care planning and empower patients to make informed decisions about their end-of-life care.
Frequently Asked Questions (FAQs)
- What is the difference between euthanasia and physician-assisted suicide?
-
Euthanasia involves a physician actively ending a patient’s life, while physician-assisted suicide involves a physician providing the means for a patient to end their own life.
-
Is euthanasia legal in the United States?
-
Euthanasia is illegal in the United States, but physician-assisted suicide is legal in states such as Oregon, Washington, and California.
-
What are the ethical arguments against euthanasia?
-
Opponents of euthanasia argue that it violates the sanctity of life, increases the risk of abuse, and undermines trust in healthcare professionals.
-
How does euthanasia impact end-of-life care?
-
Euthanasia can influence end-of-life care by raising awareness about patient autonomy, pain management, and patient-centered care.
-
What safeguards are in place in countries where euthanasia is legal?
- Countries with legalized euthanasia have strict safeguards such as mandatory consultations, waiting periods, and documentation requirements to ensure patient safety and ethical practice.
In conclusion, the case of Jolanda Fun highlights the complexity and emotional significance of the euthanasia debate, underscoring the need for compassionate and ethical end-of-life care options. As the conversation around euthanasia continues to evolve, it is essential for society and healthcare systems to engage in thoughtful dialogue and ethical reflection to address the diverse and nuanced perspectives on end-of-life decision-making.